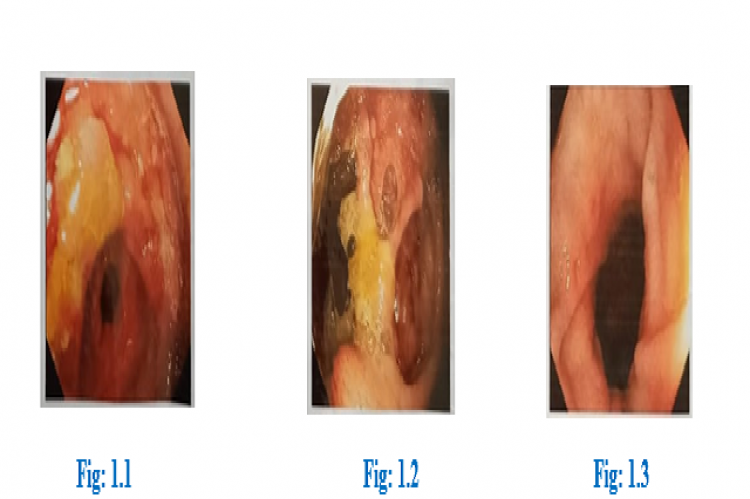
Tuberculosis (TB) is an endemic airborne disease. TB is the 13th leading cause of death and second leading infectious killer after covid 19. In worldwide, 10.6 million people suffering from TB. Abdominal TB cases make up above 3% of all extra pulmonary TB as per the Index TB Guidelines. Abdominal tuberculosis is the type of extra pulmonary tuberculosis that is TB infection of any organ in the abdominal cavity. Intestinal tuberculosis is a rare clinical manifestation of extra pulmonary TB. Intestinal tuberculosis is a rare clinical manifestation of extra pulmonary TB. A 63 year old female patient was admitted with complaints of fatigue for one week. She has fever for one month on and off with significant loss of weight and had recent history of deep vein thrombosis (DVT). Now she was newly detected with type 2 diabetes mellitus too. CECT scan of abdomen and pelvis was performed with finding of wall thickening of cecum and terminal ileum, mild splenomegaly, multiple adjacent enhancing mesenteric nodes, multiple enlarged enhancing conglomerated para aortic, retroperitoneal and common iliac nodes, multiple short discontinuous segments of bowel wall thickening with luminal narrowing involving ascending, transverse and descending colon. A detailed examination of colonoscopy concluded intestinal tuberculosis. Although Expert MTB/RIF ultra-extrapulomonary showed MTB not detected as well as the rifampicin resistance not detected. MTB treatment was initiated. After the drug had taken which resulted in hepatitis that is, ATT induced hepatitis. Therefore the particular drug had stopped and alternative was started. This case points outs the diagnostic challenges of intestinal tuberculosis and commonly caused anti tubercular agent induced hepatotoxicity. In this case it takes time to find out the disease condition and after starting the TB drugs which leads to hepatotoxicity. This further leads to the elongation of the treatment duration.
View:
- PDF (536.31 KB)